Moles are the most common indication of melanoma and other skin cancers; luckily, they can be kept track of with skin self-examinations. According to the National Cancer Institute, those with more than 50 common moles have an increased chance of developing melanoma (“Common Moles, Dysplastic Nevi, and Risk of Melanoma”), which is why it is important to self-examine your skin (and your loved one’s skin!) every month.
There are no hard and fast visual rules about which moles might and might not develop into melanoma, however there are some guidelines you can follow when self-examining your skin to judge if any of your moles should be checked out by a physician.
Firstly, there are two kinds of moles. Common moles are, as the name suggests, common and less likely to develop into skin cancer (even though instances of common moles developing into melanoma do occur). The other kind of mole, the dysplastic nevus (plural nevi), has an abnormal appearance in comparison to the common mole. While dysplastic nevi are more likely to develop into skin cancer than common moles are, dysplastic nevi are not a definite sign of skin cancer. However, it is important to pay particular attention to changes in dysplastic nevi during your self-examinations.
Check out our page Skin Check Guide for more information!
The National Cancer Institute recommends that you look for the following changes in both common moles and dysplastic nevi, and to see a physician if any one of them occurs:
- The color changes
- It gets smaller or bigger
- It changes in shape, texture, or height
- The skin on the surface becomes dry or scaly
- It becomes hard or feels lumpy
- It starts to itch
- It bleeds or oozes
(“Common Moles, Dysplastic Nevi, and Risk of Melanoma”. National Cancer Institute)
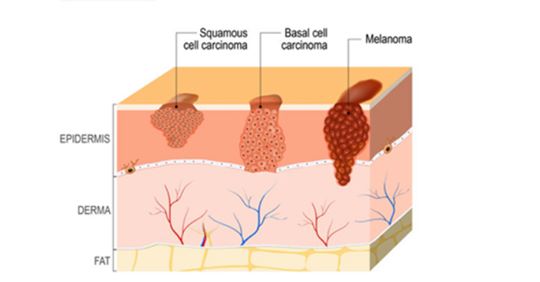
In addition to these changes, there are some more obvious signs that a mole may be developing into melanoma. Be aware that there are several types of melanoma and skin cancer, which manifest in disparate ways; it is important to track all changes on your skin, even if they do not appear to be indicative of melanoma. A good rule to follow here is the ABCDE’s of early melanoma detection, which the National Cancer Institute identifies as the following:
- Asymmetry. The shape of one half does not match the other half.
- Border that is irregular. The edges are often ragged, notched, or blurred in outline. The pigment may spread into the surrounding skin.
- Color that is uneven. Shades of black, brown, and tan may be present. Areas of white, gray, red, pink, or blue may also be seen.
- Diameter. There is a change in size, usually an increase. Melanomas can be tiny, but most are larger than 6 millimeters wide (about 1/4 inch wide).
- Evolving. The mole has changed over the past few weeks or months.
(“Common Moles, Dysplastic Nevi, and Risk of Melanoma”. National Cancer Institute)
Tips for an effective self-examination
Now that you have an idea of what to look for, it’s important to get the most out of your monthly self-examination as possible. Here are some tips for being as thorough as possible:
- Use a full length and handheld mirror
- Perform your self-examination in a well lit area
- Have someone else check areas you can’t see
- Write down and take photos of any new discoveries, such as changes or new moles; this will be helpful if you need to contact your physician
- Remember to check often forgotten areas such as: fingernails and toenails, scalp (using a comb and/or blowdryer), the bottoms of feet and in between toes, ears, and underarms
Thank you for reading, and we hope this post encourages awareness and skin self-examinations! If you would like more information, look to one of our sources below. While the principles of self-examination are universal, be aware that not every website we source content from is Canadian.
“Common Moles, Dysplastic Nevi, and Risk of Melanoma”. National Cancer Institute. 11.01.11.
“How to Check your Skin for Skin Cancer”. National Cancer Institute. 09.16.11.
“About Melanoma: Signs and Symptoms of Melanoma”. NCCN Guidelines for Patients: Melanoma. 2014: National Comprehensive Cancer Network Foundation.




 There are several different routes to being diagnosed with melanoma. The first step is generally a physical screening, during which your physician will check your skin for moles or other abnormalities and ask questions, such as if there have been any changes in your skin or moles, or the length of time you have had certain moles. In order to accurately answer these questions, it helps to self-examine your skin monthly to keep track of any changes; more information on moles and skin self-examinations can be found
There are several different routes to being diagnosed with melanoma. The first step is generally a physical screening, during which your physician will check your skin for moles or other abnormalities and ask questions, such as if there have been any changes in your skin or moles, or the length of time you have had certain moles. In order to accurately answer these questions, it helps to self-examine your skin monthly to keep track of any changes; more information on moles and skin self-examinations can be found 






