HAVE YOU BEEN TOLD YOU HAVE A SKIN CANCER OR MELANOMA?
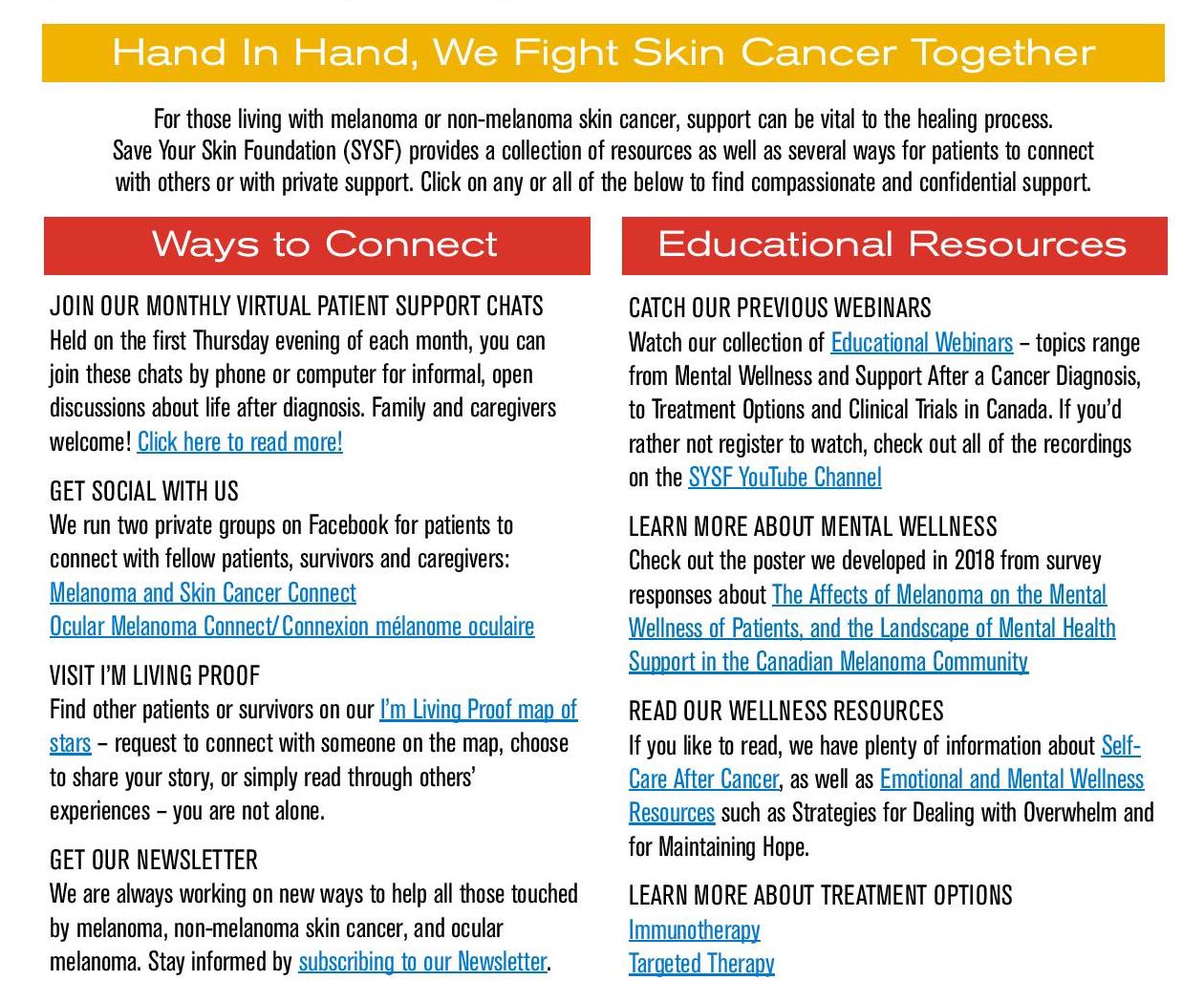
Receiving a cancer diagnosis is never easy. Arming yourself with information may help you feel more in control of the situation. Save Your Skin Foundation wishes to bring hope and support to all those newly diagnosed, currently undergoing treatment, or to those in remission. We invite all ocular melanoma, melanoma, and non-melanoma skin cancer patients, at any stage, to get in touch.
Plenty of resources are listed below, but you can always get in touch with us directly as well.
JOIN OUR MONTHLY VIRTUAL PATIENT FIRESIDE CHATS
Join our Monthly Patient Fireside Chats which have a small standing group of core hosts & new topics every first Thursday of the month. These fireside chats are for those looking for support that can be vital to the healing process.
Our monthly chats are attended by a small standing group of core hosts, including SYSF Founder Kathy Barnard and fellow survivors, who take turns leading the group in a themed topic each month, allowing plenty of time for questions and discussion. Read more>>
GET SOCIAL WITH US
We run two private groups on Facebook for patients to connect with fellow patients, survivors and caregivers:
VISIT I’M LIVING PROOF
Find other patients or survivors on our I’m Living Proof map of stars – request to connect with someone on the map, choose to share your story, or simply read through others’ experiences – you are not alone.
GET OUR NEWSLETTER
We are always working on new ways to help all those touched by melanoma, non-melanoma skin cancer, and ocular melanoma. Stay informed by subscribing to our Newsletter.
WEBINARS
Diagnosed with Skin Cancer? Here’s What To Do Next: Educational Webinar, An Hour with Kathy Barnard
 Recorded February 24, 2022
Recorded February 24, 2022
In this webinar, Kathy Barnard, founder of SYSF and melanoma survivor, shares her experience navigating and advocating through the Canadian health care system, which is complicated and can be confusing to many. She helps patients and caregivers understand how to get from diagnosis to surgical and/or systemic treatment of melanoma or non-melanoma skin cancer (NMSC) such as metastatic basal cell carcinoma (BCC), squamous cell carcinoma (SCC) or merkel cell carcinoma (MCC).
 Recorded August 5, 2020
Recorded August 5, 2020
Hear the latest updates on current immunotherapy and targeted therapy treatments for melanoma and non-melanoma skin cancers in Canada. Dr. Smylie and Dr. Iafolla present on recommended dietary and lifestyle habits while on treatment, as well as managing toxicities from fever and pneumonitis to dermatologic complications from immune checkpoint inhibitors.
 Recorded September 28, 2022
Recorded September 28, 2022
This webinar help patients understand prognostic testing when diagnosed with Ocular Melanoma. It also discusses options for health care professionals for prognostic testing, what it can mean to patients and how it can affect treatment decisions. Presenters: Katherina Alsina, PhD, Castle BioSciences and Dr. Marcus Butler, Medical Oncologist, Princess Margaret Cancer Centre
Catch our previous webinars
Watch our collection of Educational Webinars – topics range from Mental Wellness and Support After a Cancer Diagnosis, to Treatment Options and Clinical Trials in Canada. If you’d rather not register to watch, check out all of the recordings on the SYSF YouTube Channel
Read our wellness resourses
If you like to read, we have plenty of information about Self Care After Cancer, as well as Emotional and Mental Wellness Resources such as Strategies for Dealing with Overwhelm and for Maintaining Hope.
Learn more about treatment options
View Care Decision resources
Customized for the Canadian audience, these downloadable booklets, created by AIM at Melanoma and reviewed by Save Your Skin Foundation, are to support patients and help guide their decision making regarding next steps for stage III and IV melanoma:
The Doctor who gave you your diagnosis may not be the right person to treat you. Ask about their experience with the skin cancer you are diagnosed with; if they are not experienced, ask for referrals to other doctors in your area with more expertise.
You should ensure the Doctor who will help you through your journey with skin cancer is both experienced with your specific diagnosis and understands you.
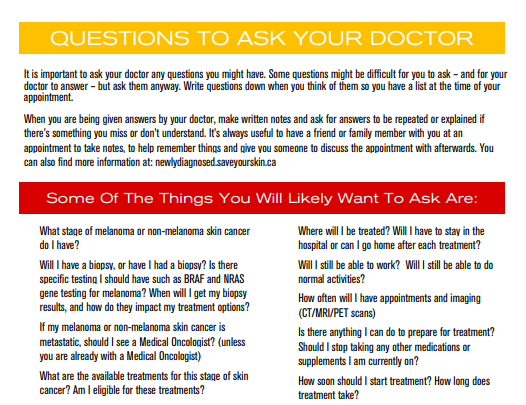
It is important to ask your doctor any questions you might have. Some questions might be difficult for you to ask – and for your doctor to answer – but ask them anyway. Write questions down when you think of them so you have a list at the time of your appointment.
When you are being given answers by your doctor, make written notes and ask for answers to be repeated or explained if there’s something you miss or don’t understand. It’s always useful to have a friend or family member with you at an appointment to take notes, to help remember things and give you someone to discuss the appointment with afterwards.
Some of the things you will likely want to ask about are:
- What stage of melanoma do I have?
- What are the available treatments for this stage of melanoma?
- Will I have more than one treatment?
- What are the risks and benefits of each treatment for melanoma?
- Will my age, stage of melanoma, and other health conditions limit my treatment choices?
- Do I have to get treated?
- Where will I be treated? Will I have to stay in the hospital or can I go home after each treatment?
- What can I do to prepare for treatment? Should I stop taking my medications?
- How soon should I start treatment? How long does treatment take?
- How much will the treatment cost? How can I find out how much my insurance company will cover?
- How likely is it that I’ll be cancer-free after treatment?
- What symptoms should I look out for while being treated for melanoma?
- When will I be able to return to my normal activities?
- What is the chance that the melanoma will come back or spread?
- What should I do after I finish treatment?
Click HERE for a full list of suggested questions and resources you can download and print to take with you to your appointments.
Click HERE for a fillable PDF checklist you can work through with your physician. A printable version is also available.
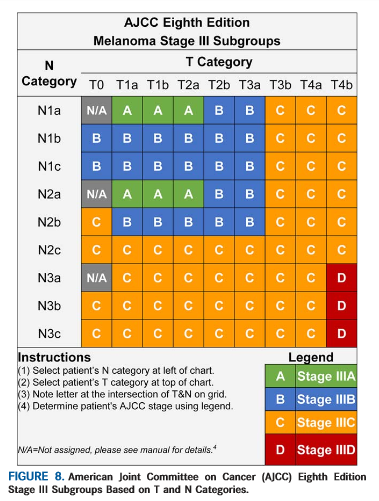
Staging is commonly used in melanoma diagnosis and treatment to indicate the advancement and severity and cancer in a patient. Melanoma stages range between 0-IV based on the TNM (tumour, nodes, metastasis) system. The TNM system is dictated by the size of the primary (first) tumour, the occurrence of cancer cells in the surrounding lymph nodes, whether the cancer has metastasized (spread to other regions in the body), and whether there is ulceration (if there is ulceration, the skin covering the melanoma cannot clearly be seen). While these figures can be intimidating in the later stages, the staging system is imperative for dictating the treatment process a patient will undergo.
Stage 0 is thin melanoma which has not penetrated (invaded) the deeper layers of the skin (in situ).
Stages I and II are melanomas that are limited to the skin. These melanomas vary in how thick they are and whether the skin covering the melanoma is ulcerated or not. Thicker melanomas and ulcerated melanomas have a higher risk of recurring.
Stage III is melanoma that has spread from the original site of your melanoma to 1 or more of the nearby lymph nodes or to the nearby skin/tissue in between. Stage III melanoma is divided into 4 groups, A, B, C, and D.
Stage IV is melanoma that has spread farther than regional lymph nodes, to distant sites such as the lung, liver, or brain.
While staging is clearly a complicated process with many variables, it is important to understand why a particular cancer case has been given its stage, and what that means for the future treatment of that patient.
Click here to view additional resources: https://www.patientresource.com/Melanoma_Staging.aspx
Works Cited Above:
“Melanoma Staging”. NCCN Guidelines for Patients: Melanoma. 2014: National Comprehensive Cancer Network Foundation.
Canadian Cancer Society, “Stages of Melanoma“.
There are several treatments for skin cancer. Your melanoma diagnosis, age, location, and general health are some of the factors that should be taken into account when you are considering your options. Treatments exist in the following broad categories that could be tailored to fit your needs:
SURGERY
In certain cases it is possible to operate and physically remove the cancer tumours. This is not always an option.
IMMUNOTHERAPY
This is a new drug treatment area in which the immune system is enhanced so the body can fight off cancer in the way it fights more common ailments. Learn more
TARGETED THERAPY
A treatment that interferes with specific molecules involved in the growth and spreading of cancers, inhibiting the development the cancer. Learn more
CHEMOTHERAPY
These drugs are used to treat many types of cancers by impacting the cancer cells’ ability to grow or multiply. Due to their impact on non-cancer cells, these treatments can have side effects. This is typically not used in melanoma and non-melanoma skin cancers any more.
RADIATION THERAPY
Destruction of tumours using a high-energy radiation beam.
COMBINATION THERAPY
The combination of two or more therapies.
An up-to-date list of available treatments can be found on the Canadian Agency for Drugs and Technologies in Health (CADTH) website’s Provincial drug formulary database, which can be accessed here. For more information about any and all treatments and whether they might be an option for you, ask your Doctor.
New! Our friends the Canadian Skin Patient Alliance have created a unique tool called Is My Prescription Covered? It is a first of its kind digital, interactive drug coverage finder. It is available in English and French. Click here to check it out: www.canadianskin.ca/is-my-prescription-covered
Follow-up after melanoma treatment depends on the stage of the melanoma. A melanoma diagnosis increases the risk of another melanoma. Therefore, your doctor will perform a full-body skin examination, at least every year, for the rest of your life.
Self-monitoring:
Your doctor will also teach you how to examine your skin and lymph nodes. You should examine your skin at least monthly. Make sure you check the back of your body. Use a mirror or have someone check for you. Look for changes in moles, any new growths, sores that do not heal, and abnormal areas of skin.
Contact your doctor right away if you notice any abnormalities. Your doctor may also recommend that you examine your lymph nodes every month. A schedule like the following one is followed if you have no signs or symptoms of melanoma.
If you do develop new signs or symptoms, your doctor will investigate them and determine appropriate treatment and follow-up based on your test results.
STAGE 0 (IN SITU)
Your doctor will perform a full-body skin examination at least every year. You should examine your skin every month.
STAGE IA
Your Dermatologist will see you on the following schedule to create a history and perform a physical examination:
- Every three to twelve months for five years
- Once a year after that
Also, at least every year, your doctor will perform a full-body skin examination. You should examine your skin and lymph nodes every month.
STAGE IB, IIA, IIB, IIC
Your Dermatologist will see you on the following schedule to take a history and perform a physical examination:
- Every three to six months for two years
- Every three to twelve months for two years
- Once a year after that
Your doctor may decide to perform selected investigations, such as blood tests or imaging studies every six to twelve months, to screen for tumour recurrence or spread.
Also, at least every year, your doctor will perform a full-body skin examination. You should examine your skin and lymph nodes every month.
STAGE IIIA, IIIB, IIIC, IV
Treatment of stage III melanoma and beyond will be performed by an Oncologist.
Physical examination (skin examinations, chest x-rays, CT scans of trunk, pelvis, and head)
- Year 1: every three months
- Year 2 : every four months
- Years 3-5: at least every six months
- Annually after five years
New treatments are tested in clinical trials before they are approved for general use. There are safeguards in place to ensure clinical trials are as safe as possible and meet medical ethical standards. Participating in a trial can be a way to have access to potentially helpful new therapies you couldn’t get any other way.
Clinical trials are funded by pharmaceuticals evaluating their new treatments. Therefore, the treatments, tests, and doctor visits are usually paid for and patients are followed very carefully. Clinical trials usually have very specific criteria for the patients who can participate, such as severity or stage of disease and whether and what types of previous treatments you have had.
Please click here to see our “About Clinical Trials” page for more information about clinical trials, or for help finding a clinical trial that may be right for you.
If you are interested in participating in a clinical trial, ask your doctor if there are any appropriate studies available to you.
NOTE: The information on the Save Your Skin website is not intended to replace the medical advice of a doctor or healthcare provider. While we make every effort to ensure that the information on our site is as current as possible, please note that information and statistics are subject to change as new research and studies are published.
100% OF DONATIONS GO TO PATIENTS
Making awareness and education available is crucial. Since 2006, the Foundation has worked to raise awareness of melanoma and non-melanoma skin cancers focusing on education, prevention and the need for improved patient care.