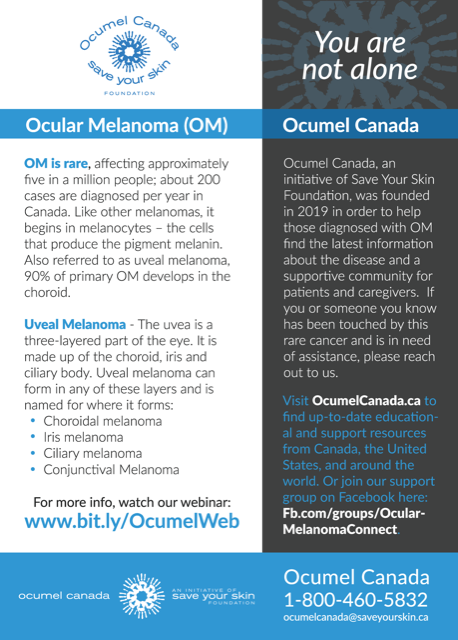
Ocular melanoma is rare, affecting approximately five in a million people; about 200 cases are diagnosed per year in Canada. Like other melanomas, it begins in melanocytes – the cells that produce the pigment melanin that colours the skin, hair, and eyes, as well as forms moles. While it represents only 5% of melanomas, ocular melanoma is rapid and aggressive, accounting for 9% of melanoma deaths. Also referred to as uveal melanoma, ocular is a more inclusive term; 90% of primary ocular melanoma develops in the choroid.
There are no established risk factors for ocular melanoma, but it often occurs in blue-eyed, fair-skinned people over sixty years old. Treatment can be successful if the tumours in the eye are caught early. Around 50% of tumours will metastasize, usually in two to five years. Metastasis is to the liver in approximately 90% of these cases, but can also occur in the lungs, bones, brain or abdomen.
WEBINAR RECORDING AVAILABLE, CLICK HERE TO VIEW:
And click here to view an interactive e-book by CureOM:
For more information about ocular melanoma, please click on the following links to download-able documents we have created with the permission of CureOM, an initiative of Melanoma Research Foundation. Thank you to the team at CureOM for their inspiration and support:
Different types of Melanoma of the eye include:
Uveal Melanoma The uvea is three-layered part of the eye. It is made up of the choroid, iris and ciliary body. Uveal melanoma can form in any of these layers and is named for where it forms:
Choroidal melanoma begins in the layer of blood vessels – the choroid – beneath the retina. It is the most common type of uveal melanoma. A 2012 article by the American Academy of Ophthalmology discusses the differences between choroidal nevi and choroidal melanoma.
Iris melanoma occurs in the front, colored part of the eye. Iris melanomas usually grow slowly and do not typically metastasize, or spread, to other parts of the body outside the eye.
Ciliary melanoma occurs in the back part of the eye – in the ciliary body. Melanomas in the ciliary body tend to grow and metastasize to the liver more quickly than iris melanomas.
Conjunctival Melanoma The conjunctiva is the clear tissue that covers the white part of the eye, as well as the inside of the eyelids. Conjunctival melanoma is very rare. It often appears as a raised tumor and may contain little or even no pigment. Conjunctival melanoma most commonly occurs in the bulbar conjunctiva – the mucous membrane that covers the outer surface of the eyeball. Unlike other forms of ocular melanoma that spread most often to the liver, when conjunctival melanoma spreads, it most often spreads to the lungs.
Works cited: “Types of Ocular Melanoma”, CureOM.org
Members of your Medical Team may include an Ophthalmologist, a Medical Oncologist, and/or a Radiation Oncologist. An Ophthalmologist is an eye doctor and will be able to inform you about the appropriate treatments for the primary tumour in the eye. A Medical Oncologist deals with issues of metastasis, prognosis, and existing and experimental therapies that may treat or prevent the appearance of the melanoma. A Radiation Oncologist deals with radiation treatment. In some cases, this might treat the eye itself, in others it might treat some of the melanoma that has spread.
You should ensure the Doctor who will help you through your journey with ocular melanoma is both experienced with your specific diagnosis, and understands you. Sometimes that means getting a second opinion. The Doctor who gave you your diagnosis may not be the right person to treat you. Ask about their experience with the cancer you are diagnosed with; if they are not experienced, ask for referrals to other doctors in your area (or sometimes farther away) with more expertise.
Feel free to look around this website for more information and resources to help you. For example, visit our page Self Care After Cancer for a list of questions to ask your medical team, subscribe to our SYSF newsletter to stay up to date on Ocumel Canada news, or join our monthly Patient/Caregiver Support virtual meetings to connect with others. You can also click here to read one metastatic ocular melanoma survivor’s experienced perspective and direct guidance on the current landscape of options in ocular melanoma treatment in Canada: Opening Our Eyes To Ocular Melanoma
For additional information, please visit our pages listed here, which contain up-to-date links to resources and articles, research, and news about uveal/ocular melanoma:
Additional Resources and Support
And anytime, you can contact us at ocumelcanada@saveyourskin.ca or 1-800-460-5832
Click on the image below to meet other OM patients, survivors and caregivers by joining our closed Facebook group, Ocular Melanoma Connect:
NOTE:The information on the Save Your Skin Foundation website is not intended to replace the medical advice of a doctor or healthcare provider. While we make every effort to ensure that the information on our site is as current as possible, please note that information and statistics are subject to change as new research and studies are published.
Making awareness and education available is crucial. Since 2006, the Foundation has worked to raise awareness of melanoma and non-melanoma skin cancers, and ocular melanoma, focusing on the need for improved patient care.