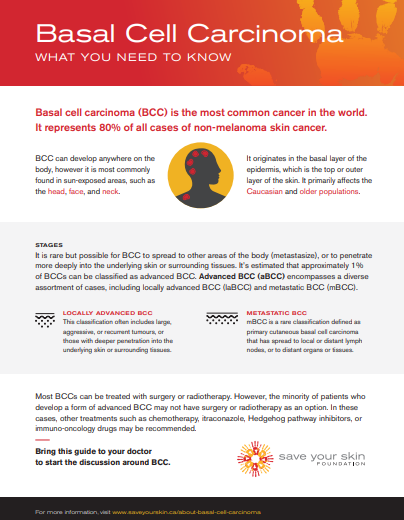
BCC is the most common cancer in the world, with incidence exceeding that of all other cancers combined.
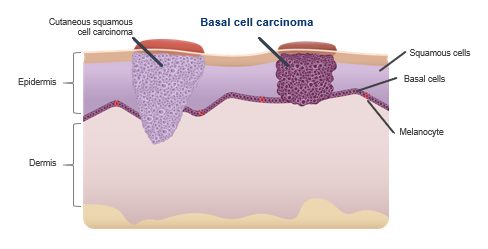
BCC represents approximately 80% of all cases of non-melanoma skin cancer (NMSC), and predominantly affects the Caucasian and older population. BCC originates in the basal layer of the epidermis, with studies so far suggesting origins primarily being from stem cells. (Peterson SC, et al. Cell stem cell 16.4 (2015): 400-412; Sehgal VN, et al. Skinmed 12.3 (2014): 176-81)
BCC can develop anywhere, though it is most commonly found in sun exposed areas. It is possible to have more than one BCC. It is rare but possible for BCC to spread, or metastasize – it is estimated that ~1% of BCCs can be classified as advanced BCC. (Mohan SV & Chang ALS. Curr Derm Rep 2014;3:40–5)
Helen’s Story
“Basal cell carcinoma, in general, is the most common form of skin cancer in the world,” says Dr. Vanessa Bernstein, BC Cancer Agency. “One in eight Canadians will develop it during their lifetime. But the majority of the cases of basal cell cancer won’t be locally advanced or metastatic. These 99 per cent of basal cell cancers will be treated with local options like surgery or radiation, and they’ll be cured most of the time by that. Helen’s is an unusual case because her advanced basal cell cancer is quite a rare form of what’s usually a slow-growing, common skin cancer. It came back after radiation and it kept recurring after treatment, which is when we knew we were in trouble.”
Click here to read the full story: It Takes a Village to Stand Up to Cancer
Advanced BCC (aBCC)
Advanced BCC encompasses a heterogeneous assortment of cases, including metastatic BCC as well as locally advanced BCC (for which no formal definition exists but which generally includes large, deep, aggressive, or recurrent tumors).
Most BCCs can be effectively treated with standard surgical excision, Mohs micrographic surgery, curettage and electrodessication, radiotherapy, and/or superficial field therapies (including 5-fluorouracil, imiquimod, and photodynamic therapy); however, a minority of patients develop advanced BCC.
Locally advanced BCC (laBCC)
In general, this classification often includes large, aggressive, or recurrent tumors or those with deeper penetration into the underlying skin and surrounding tissues.
LaBCC may be broadly categorized as cases for which (further) surgery is considered inappropriate (i.e., would be substantially disfiguring, may cause significant morbidity, loss of function), and radiation is considered inappropriate as a single modality or second-line treatment.
Metastatic BCC (mBCC)
Metastatic BCC is defined as primary cutaneous basal cell carcinoma that has spread to local or distant lymph nodes or to distant organs or tissues.
Migden, et al. Cancer Treatment Reviews 64 (2018) 1–10; 2. Mohan SV & Chang ALS. Current dermatology reports 3.1 (2014): 40-45
BCC can be classified into indolent or aggressive subtypes:
Indolent subtypes
Nodular and superficial are the most common indolent subtypes of BCC. Nodular BCC, the most common histological subtype of BCC, predominates on the head, especially the cheeks, nasolabial folds, forehead, and eyelids. Superficial BCC, the second most common histological subtype, is frequently found on the trunk and extremities.
Aggressive subtypes
Aggressive subtypes such as morpheaform, micronodular, infiltrative, and mixed histologies that are estimated to comprise 5–15% of BCC. They show the deeper invasion of tissues and a higher rate of recurrence. Frequently found on the head and neck.
Marzuka AG & Book SE. The Yale journal of biology and medicine 88.2 (2015): 167-179.
Treatment Pathway
In March 2022 Health Canada approved Libtayo® (cemiplimab) for patients with locally advanced basal cell carcinoma (LaBCC), previously treated with a hedgehog pathway inhibitor (HPI).
Real-world data indicate that the majority of aBCC patients who progress on or are intolerant to HPIs are managed with surgery or radiotherapy (36%-65%). Other treatment options include HPIs, itraconazole, chemotherapy, or Libtayo® (cemiplimab).
For more information please click below to watch our September 2020 webinar titled Basal Cell Carcinoma: What Patients Need to Know
Videos
Basal Cell Carcinoma: What Patients Need to Know
September 29, 2020
Dr. Max Sauder, Onco-dermatologist at Princess Margaret Cancer Centre, reviews the latest news, clinical data and other updates as they relate to the treatment of cutaneous basal cell carcinoma (BCC), a common and sometimes metastatic skin cancer. Dr. Sauder provides an update on skin cancer statistics in Canada, the science behind primary and metastatic BCC diagnosis and treatment, and shares his key insights into what the landscape of metastatic BCC immuno-oncology treatment looks like for the near future in Canada.
Video: What is Basal Cell Carcinoma (BCC)
Sept 13, 2016
Additional Resources
NOTE: The information on the Save Your Skin website is not intended to replace the medical advice of a doctor or healthcare provider. While we make every effort to ensure that the information on our site is as current as possible, please note that information and statistics are subject to change as new research and studies are published.
MONTHLY SELF-EXAMS ARE KEY TO EARLY DETECTION
Making awareness and education available is crucial. Since 2006, the Foundation has worked to raise awareness of melanoma and non-melanoma skin cancers focusing on education, prevention and the need for improved patient care.