Melanoma begins as a malignant tumour in the melanocytes, which are the cells that produce melanin or pigment. As a malignant cancer, melanoma can metastasize to other parts of the body. There are several subtypes of melanoma, including cutaneous, acral, mucosal, ocular melanoma, and even amelanotic melanoma.
To read more about melanoma diagnosis and staging, treatment options, patient and caregiver support, questions to ask your doctor, and more, visit our After Diagnosis page.
There are different types of melanoma
There are four different types of cutaneous melanoma, which are determined by microscopic examination of a biopsy sample.
- Superficial Spreading Melanoma counts for approximately 70% of melanomas of the skin. Superficial spreading melanoma usually develops from an atypical mole and can be found anywhere on the body.
- Nodular melanoma makes up about 10-15% of melanomas. Nodular melanoma starts growing down into the skin and spreading quickly.
- Lentigo maligna melanoma makes up about 10-15% of melanomas. Lentigo maligna melanoma is most often seen on skin that has been exposed to the sun. These spots are often large.
- Acral lentiginous melanoma (ALM) is a type of cutaneous melanoma. Its name comes from the Greek word for “extremity” and refers to the fact that ALM is found on the palms of the hands, the soles of the feet, or under the nails. Though not very common in the general population, ALM is the most common type of melanoma in people with darker skin and those of Asian descent. Up to 60 – 75% of melanoma in people of colour occurs on the palms of the hands, soles of the feet and the nail areas.The risk factors for acral melanomas are not fully understood, but sun is less likely to be a factor. Because of the misconceptions that melanomas only occur in sun-exposed areas and that people of color are not at risk for melanoma, these melanomas are often discovered later than other types, which can lead to a worst prognosis.
Mucosal melanoma develops in the lining of the respiratory, gastrointestinal, and genitourinary tracts. It is a rare form of melanoma, making up only about 1% of melanoma cases and is often diagnosed at an advanced stage in the elderly. Approximately 50% of mucosal melanomas begin in the head and neck region, 25% begin in the ano-rectal region, and 20% begin in the female genital tract. The remaining 5% occur in the esophagus, gallbladder, bowel, conjunctiva, and urethra.
More information about mucosal melanoma can be found on the Melanoma Research Foundation website.
A seven-point checklist for moles is useful in identifying lesions that need to be excised. The three major signs are change in shape, change in size and change in colour; the four minor signs are over 7 mm in diameter, inflammation, crusting or bleeding and minor irritation or itch. Lesions with any major signs or three minor signs are suspicious of melanoma. Unfortunately malignant melanoma can present atypically.
About 2% of all melanomas are amelanotic. Amelanotic melanoma is the subtype most often reported as simulating other cutaneous lesions, but even pigmented melanomas are commonly misdiagnosed—especially as melanocytic naevus, basal cell carcinoma, seborrhoeic keratosis or lentigo.
Any changing or atypical mole or non-healing skin lesion should be referred urgently to a dermatologist or to a surgeon with a special interest in pigmented lesions. Early detection of malignant melanoma is essential since survival prospects are strongly related to tumour (Breslow) thickness at the time of diagnosis. The Breslow thickness, measured on histological examination, is the distance between the overlying epidermal granular layer and the deepest invasive area of the primary lesion.
Source: JRSM, “Atypical melanoma”
Ocular melanoma is rare, affecting approximately five in a million people. While it represents only 5% of melanomas, ocular melanoma is rapid and aggressive, accounting for 9% of melanoma deaths.
We have expanded our resources and support for patients with ocular melanoma by creating the initiative Ocumel Canada.
Please click here to see all of the resources we have compiled: About Ocular Melanoma
Understanding your Pathology Report – Webinar Recording Available:
To diagnose diseases such as cancer, a sample of tissue called a biopsy is taken from a patient and examined by a pathologist to determine if cancer is present. A pathologist will then examine specimens removed during surgery (resections) for conditions such as cancer, to determine whether the tumour is benign or cancerous, and if cancerous, the exact cell type, grade and stage of the tumour. The pathologist, who is a member of your medical team, writes the pathology report that your treating doctor uses to provide the best care for you as a patient. In this webinar, Dr. Alan Spatz provides insight on understanding your pathology report so that you can play an active role in your treatment.
Click here to view the recording on youTube. With Dr. Alan Spatz, MD Director, Pathology Department, Jewish General Hospital & Professor, Pathology and Oncology, McGill University
Click here to view additional educational webinars in our video resource library: https://saveyourskin.ca/webinars-video-resources/
Melanoma Staging
Staging is commonly used in melanoma diagnosis and treatment to indicate the advancement and severity and cancer in a patient. Melanoma stages range between 0-IV based on the TNM (tumour, nodes, metastasis) system. The TNM system is dictated by the size of the primary (first) tumour, the occurrence of cancer cells in the surrounding lymph nodes, whether the cancer has metastasized (spread to other regions in the body), and whether there is ulceration (if there is ulceration, the skin covering the melanoma cannot clearly be seen). While these figures can be intimidating in the later stages, the staging system is imperative for dictating the treatment process a patient will undergo.
Stage 0 is thin melanoma which has not penetrated (invaded) the deeper layers of the skin (in situ).
Stages I and II are melanomas that are limited to the skin. These melanomas vary in how thick they are and whether the skin covering the melanoma is ulcerated or not. Thicker melanomas and ulcerated melanomas have a higher risk of recurring.
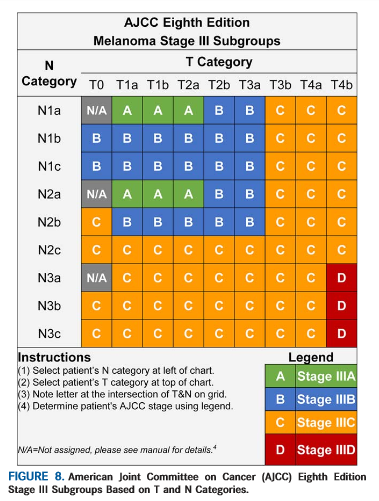
Stage III is melanoma that has spread from the original site of your melanoma to 1 or more of the nearby lymph nodes or to the nearby skin/tissue in between. Stage III melanoma is divided into 4 groups, A, B, C, and D.
Stage IV is melanoma that has spread farther than regional lymph nodes, to distant sites such as the lung, liver, or brain.
While staging is clearly a complicated process with many variables, it is important to understand why a particular cancer case has been given its stage, and what that means for the future treatment of that patient.
Click here to view additional resources: https://www.patientresource.com/Melanoma_Staging.aspx
Works Cited Above:
“Melanoma Staging”. NCCN Guidelines for Patients: Melanoma. 2014: National Comprehensive Cancer Network Foundation.
Canadian Cancer Society, “Stages of Melanoma“.
Targeted and Immunotherapy Treatments
There are several treatments for skin cancer, including targeted therapy and immunotherapy. A patient’s melanoma diagnosis, age, location, and general health are some of the factors that should be taken into account when considering treatment options.
To determine if targeted therapy is an option for a patient, their tumor must be tested for a marker called BRAF. If the BRAF test shows that the tumor has the BRAF mutation, they are eligible for targeted therapy. But if the tumor does not have the BRAF mutation, they are not eligible for targeted therapy. About half of all melanoma patients have a mutated form of code for the BRAF protein in their tumors. This is called having a BRAF mutation.
The second option is immunotherapy. Immunotherapy uses medications that are designed to “awaken” the body’s own immune system to help fight any remaining cancer cells and use the human body’s own immune system to fight cancer. It may be administered to patients intravenously in the chemotherapy unit of the hospital, but it is not the same as chemotherapy. A patient is eligible for immunotherapy regardless of a tumor’s BRAF status.
In collaboration with AIM at Melanoma we develop patient and health care provider resources relevant to the Canadian population:
AIM with Immunotherapy Resources for Canadian Health Care Providers
NEW! DECISION-SUPPORT TOOL FOR STAGE II MELANOMA
Our friends at AIM at Melanoma launched a new decision-making guide for stage II melanoma in August 2023. This document, which is an extended interview between oncologists Geoffrey Lim and Jason Luke, discusses staging, outlines the differences between different surgical and adjuvant care options, and offers insight to the kind of factors patients need to weigh when making their care plans.
Please note that this document is written for an American audience, so some content might be less relevant to Canadians.
Options for Stage II Melanoma Cancer: Making the Decision That’s Right for You
DECISION-SUPPORT TOOL FOR STAGE III MELANOMA
Customized for the Canadian audience, this pamphlet is a document to provide/discuss with patients that helps guide their decision making regarding next steps for stage III melanoma. Reviewed by Save Your Skin Foundation, updated February 2021:
Want to learn how to use the Stage III Decision-Support Tool? Peruse frequently asked questions about Stage III melanoma and learn how to use the support tool to guide your decision making. Also developed in collaboration with Save Your Skin Foundation, updated February 2021:
DECISION-SUPPORT TOOL FOR STAGE IV MELANOMA
Customized for the Canadian audience, this pamphlet, created by AIM at Melanoma and reviewed by Save Your Skin Foundation in March 2023, is a document to support patients and help guide their decision making regarding next steps for stage IV melanoma:
The document addresses:
– Stage IV melanoma clinical picture, biomarkers and pathology, and disease and patient factors involved in decision making
– Efficacy, safety, administration, and family-planning aspects of targeted therapies, immune checkpoint inhibitors, and other therapies used for stage IV melanoma
Additional Information
An up-to-date list of available treatments can be found on the Canadian Agency for Drugs and Technologies in Health (CADTH) website’s Provincial drug formulary database, which can be accessed here.
Find additional information here:
Watch our informative video about melanoma here
Click here to view and download the NCCN Guidelines for Patients – Melanoma
Medical News Today: How skin cancer becomes invasive
Source: Canadian Cancer Society, “What is Melanoma?“
Canadian Cancer Statistics
NEW! April 2022: Canadian Cancer Society Statistics Report 2021 Recap
October 16, 2019: Melanoma Statistics – A Distillation from the 2019 Canadian Cancer Society Report And a Quick Reference: Canadian Melanoma Statistics 2019
September 2018: 2018 Canadian Melanoma Statistics
June 2017: A Distillation of Melanoma Statistics, from the Canadian Cancer Society Documents Canadian Cancer Statistics 2017 and 2016.
To read the full reports on Canadian Cancer Statistics, produced by Canadian Cancer Society, Statistics Canada, Public Health Agency of Canada, Provincial/Territorial Cancer Registries, click here for past reports.
NOTE: The information on the Save Your Skin website is not intended to replace the medical advice of a doctor or healthcare provider. While we make every effort to ensure that the information on our site is as current as possible, please note that information and statistics are subject to change as new research and studies are published.
Together We Can Make A Difference
Making awareness and education available is crucial. Since 2006, the Foundation has worked to raise awareness of melanoma and non-melanoma skin cancers focusing on education, prevention and the need for improved patient care.