Melanoma on the eye, also known as ocular melanoma, is a rare but serious form of cancer that develops from melanocytes, the cells responsible for producing melanin. This pigment gives color to the eyes, skin, and hair. In this blog post, we’ll delve into the types of ocular melanoma, its diagnosis, and available treatment options. [1]
Types of Ocular Melanoma
Ocular melanoma includes ocular melanoma, also called uveal melanoma, and conjunctival melanoma. [2]
Ocular/Uveal Melanoma
The uvea is a three-layered part of the eye. It is made up of the choroid, iris and ciliary body. Uveal melanoma can form in any of these layers and is named for where it forms:
- Choroidal melanoma begins in the layer of blood vessels – the choroid – beneath the retina. It is the most common type of uveal melanoma. A 2012 article by the American Academy of Ophthalmology discusses the differences between choroidal nevi and choroidal melanoma.
- Iris melanoma occurs in the front, colored part of the eye. Iris melanomas usually grow slowly and do not typically metastasize, or spread, to other parts of the body outside the eye.
- Ciliary melanoma originates in the ciliary body, situated in the front of the uvea, responsible for secreting aqueous humor into the eye. These melanomas may grow anteriorly, visible on biomicroscopy as a darkly pigmented mass behind the pupil. Pigmentation can vary. Notably, ciliary melanomas tend to progress more rapidly, with a higher likelihood of metastasizing to the liver, compared to iris melanomas.
Treatment for ocular melanoma may involve procedures such as radioactive plaques, proton beam therapy, or even eye removal.
Recent advancements, such as the Health Canada approval of Kimmtrak in June 2022, provide hope for patients with unresectable or metastatic uveal melanoma.
Conjunctival Melanoma
The conjunctiva is the clear tissue that covers the white part of the eye, as well as the inside of the eyelids. Conjunctival melanoma is very rare. It often appears as a raised tumor and may contain little or even no pigment. Conjunctival melanoma most commonly occurs in the bulbar conjunctiva – the mucous membrane that covers the outer surface of the eyeball. Unlike other forms of ocular melanoma that spread most often to the liver, when conjunctival melanoma spreads, it most often spreads to the lungs.
Individuals diagnosed with conjunctival melanoma may undergo resection, cryotherapy, topical chemotherapy, or radiation as part of their treatment plan.
Diagnosis and Prognosis Melanoma on the Eye
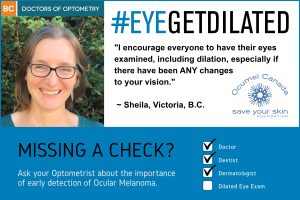
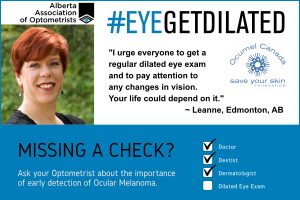
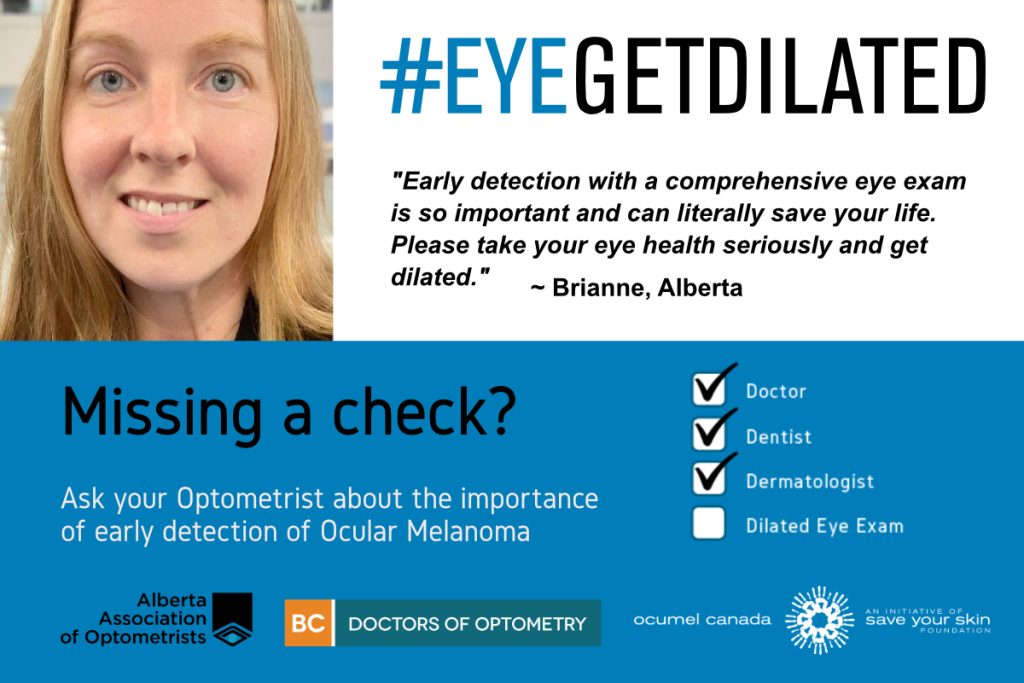
Diagnosing ocular melanoma often involves routine eye exams, where some cases may be asymptomatic. The prognosis varies, with uveal melanoma recurrence occurring in less than 5% of cases after primary treatment. However, approximately 50% of people with uveal melanoma may develop metastases, typically in the liver. [3]
Treatment Options
Treatment for melanoma on the eye depends on the type, location, and stage of the cancer. The aim is to control the primary tumor and prevent recurrence or metastasis. In advanced cases, a range of treatments, including immunotherapy, molecularly targeted agents, and liver-directed therapies, may be employed.
Ocular melanoma, though rare, poses unique challenges in diagnosis and treatment. Collaborative efforts between patients, healthcare professionals, and researchers are crucial for advancing our understanding and developing more effective treatments. Ongoing research and recent breakthroughs, such as the Health Canada approval of Kimmtrak, offer hope for improved outcomes in the fight against ocular melanoma.
[1] “Cancerous Tumours of the Eye.” Canadian Cancer Society, cancer.ca/en/cancer-information/cancer-types/eye/what-is-eye-cancer/cancerous-tumours. Accessed 4 Jan. 2024.
[2] “CURE OM – Melanoma Research Foundation.” Melanoma.org, 27 June 2023, melanoma.org/patients-caregivers/cure-om/. Accessed 4 Jan. 2024.
[3] “Ocular Melanoma.” AIM at Melanoma Foundation, www.aimatmelanoma.org/melanoma-101/types-of-melanoma/ocular-melanoma/. Accessed 4 Jan. 2024.











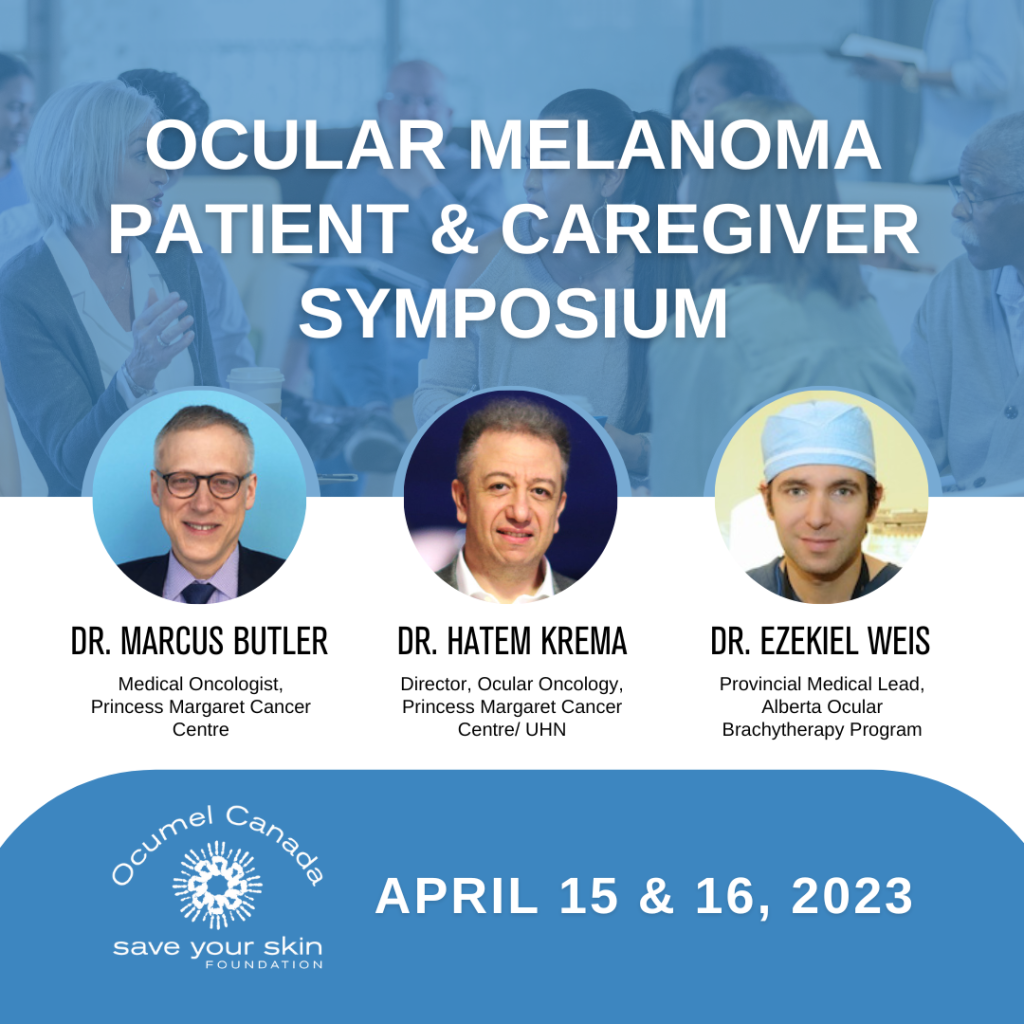

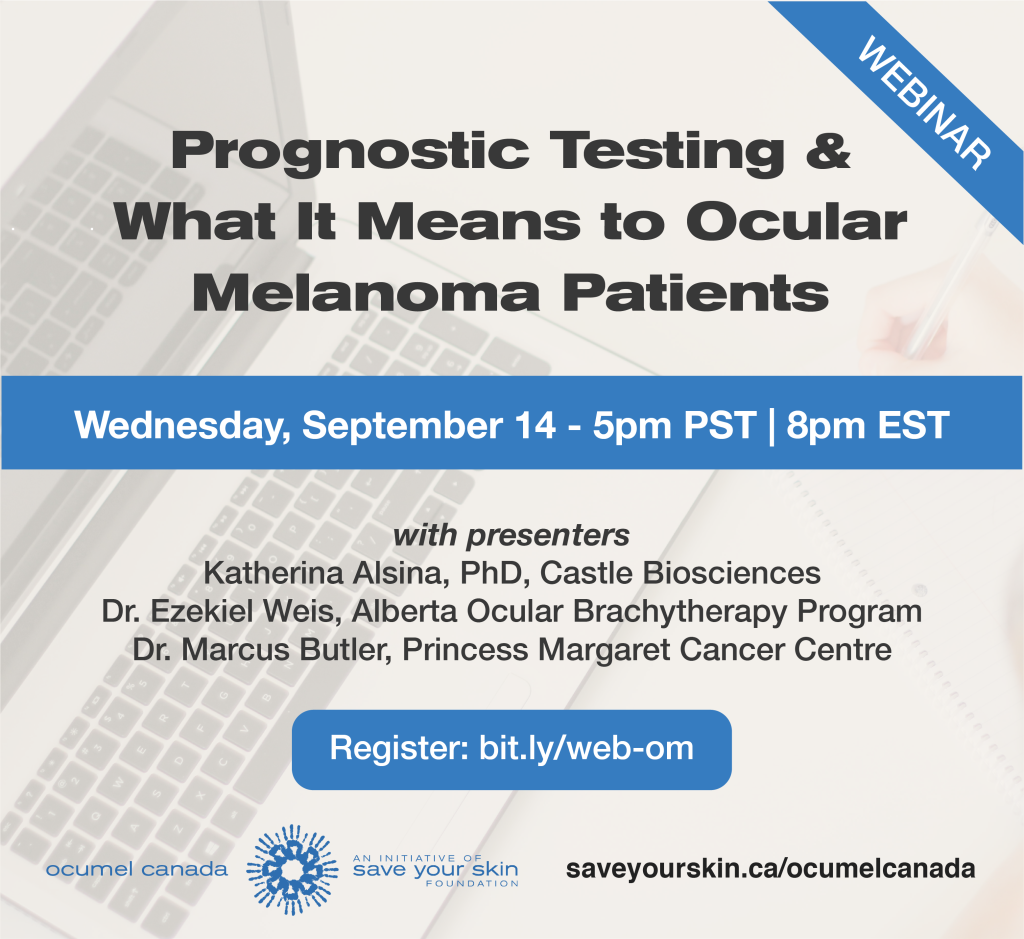 Join us for a free webinar on Wednesday, September 14 at 5pm PST | 8pm EST.
Join us for a free webinar on Wednesday, September 14 at 5pm PST | 8pm EST.
 As Ocumel Canada continues to support and advocate for patients touched by ocular melanoma (OM), we are happy to see a monumental step forward in the treatment of this disease across Canada. Last week, Health Canada granted a notice of compliance (NOC) for Kimmtrak® (tebentafusp) for the treatment of metastatic ocular melanoma, closely following approvals in the United States, Australia, and the European Union.
As Ocumel Canada continues to support and advocate for patients touched by ocular melanoma (OM), we are happy to see a monumental step forward in the treatment of this disease across Canada. Last week, Health Canada granted a notice of compliance (NOC) for Kimmtrak® (tebentafusp) for the treatment of metastatic ocular melanoma, closely following approvals in the United States, Australia, and the European Union.
 #EyePatchDay
#EyePatchDay