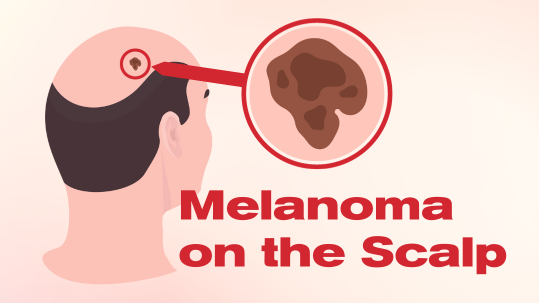
Melanoma, the most dangerous form of skin cancer, can present unique challenges when it develops on the head or neck, particularly on the scalp. In this blog post, we will look at the distinctive characteristics and considerations for melanoma on the scalp, which are crucial for effective diagnosis, treatment, and follow-up care.
Melanoma on the Scalp: Unique Characteristics and Challenges
Behavior and Treatment Differences
When melanoma occurs on the head or neck, it may behave differently than when found on other parts of the body. The complexity of the anatomy in these areas, with numerous blood vessels and lymph nodes, makes it potentially easier for melanoma to spread. As a result, treatment for melanoma on the head, neck, or scalp tends to be more aggressive.[1]
Reconstructive Surgery Considerations
Reconstructive surgery may be necessary, especially after cancer surgery on the head or neck. This can involve immediate reconstruction or a delayed approach, depending on factors like the stage of cancer and the need for additional surgeries. The waiting period allows for thorough examination and testing to determine the necessity of further procedures.
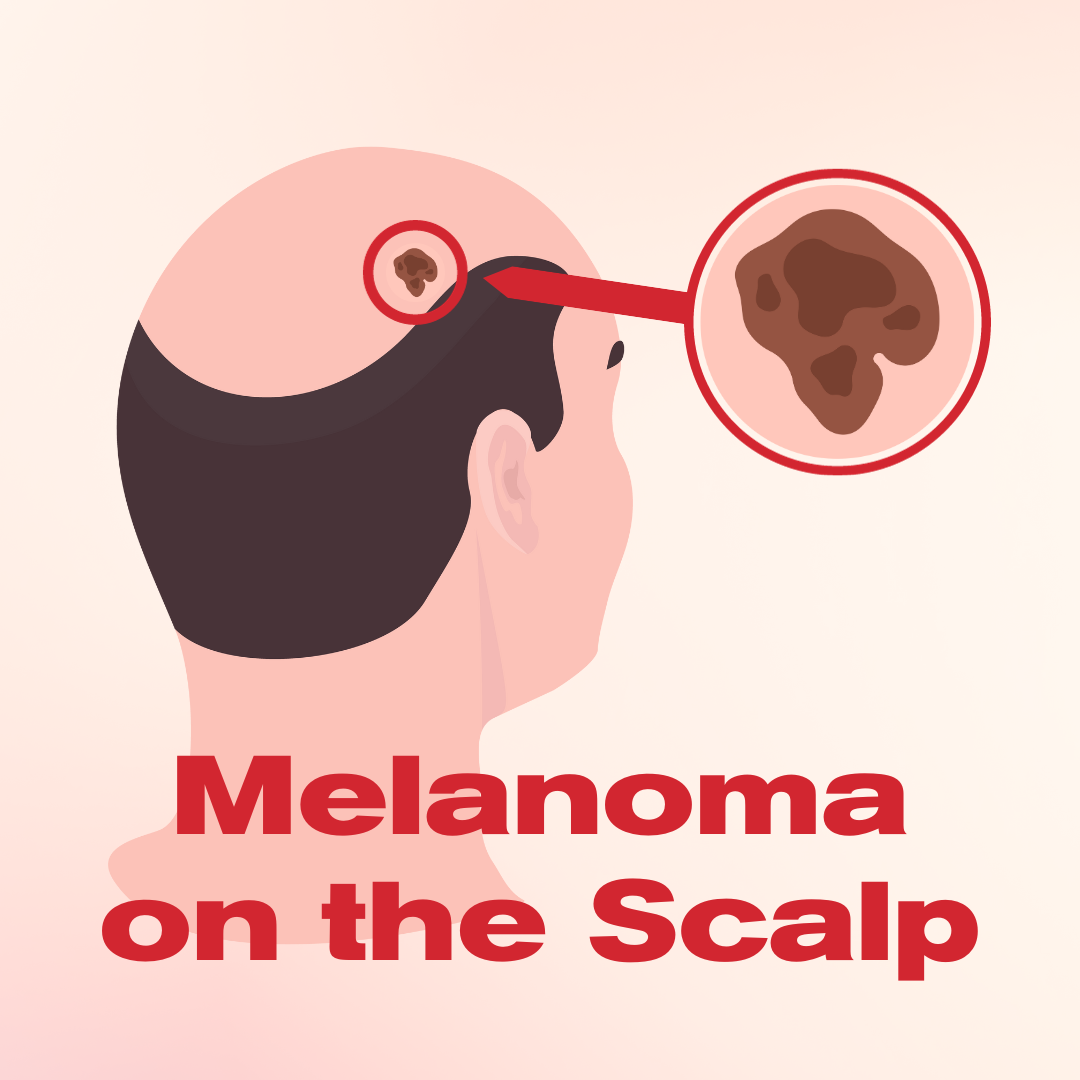
High Prevalence of Melanoma on the Scalp
Despite accounting for only 9% of the total body surface, the scalp harbors 20% of melanoma cases. A literature review highlights that scalp melanomas are more common in the elderly and men and have a 10-year survival rate of 60%.[2]
Histological Diversity and Diagnosis
Scalp melanoma encompasses a heterogeneous group of types, including lentiginous melanoma, desmoplastic melanoma, superficial spreading, and nodular melanoma. All suspicious lesions should be biopsied, with excisional biopsy often recommended.[3]
Prioritizing Awareness and Follow-Up Care
Given the aggressive nature of melanoma on the scalp, heightened awareness and proactive follow-up care are crucial. Regular check-ups, including thorough cancer examinations and relevant testing, can facilitate early detection. This, in turn, improves the chances of a positive outcome. If you suspect any unusual changes on your scalp or have concerns about melanoma, it’s essential to consult with a dermatologist promptly.
Remember, knowledge and awareness are powerful tools in the fight against melanoma, and early intervention can make a significant difference in your overall health and well-being.
Learn about other types of skin cancer:
[1] “Treatment May Differ for Melanoma on the Head or Neck.” Www.aad.org, www.aad.org/public/diseases/skin-cancer/types/common/melanoma/head-neck. Accessed 3 Jan. 2024.
[2] [3] Licata, Gaetano et al. “Diagnosis and Management of Melanoma of the Scalp: A Review of the Literature.” Clinical, cosmetic and investigational dermatology vol. 14 1435-1447. 7 Oct. 2021, doi:10.2147/CCID.S293115


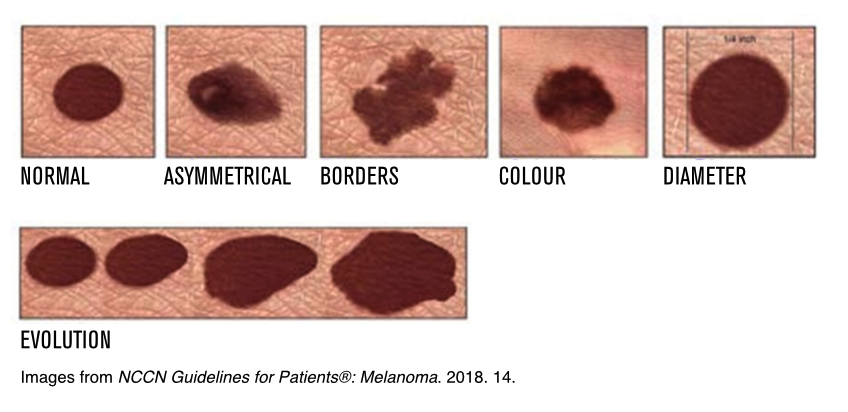 A common and effective tool to help you spot melanoma is the ABCDEs of Melanoma:
A common and effective tool to help you spot melanoma is the ABCDEs of Melanoma:







 Move for Melanoma is an activity challenge that takes place across Canada. The goal of the event is to bring awareness to melanoma, non-melanoma skin cancer and ocular melanoma, while raising funds to support patients affected with these diseases when they need it most.
Move for Melanoma is an activity challenge that takes place across Canada. The goal of the event is to bring awareness to melanoma, non-melanoma skin cancer and ocular melanoma, while raising funds to support patients affected with these diseases when they need it most.