Skin cancer is a prevalent form of cancer that affects millions of people worldwide. In Canada, about 80,000 people are diagnosed with skin cancer each year.[1] Skin cancer encompasses various types, with the most common being basal cell carcinoma (BCC), squamous cell carcinoma (SCC), and melanoma. If you or someone you know has been diagnosed with skin cancer, you may be wondering “is skin cancer curable?” The outlook for individuals with skin cancer depends on several factors, including early detection, type, stage, and treatment. Let’s explore what the experts have to say.
Early Detection is Key
According to the Cleveland Clinic, nearly all skin cancers can be cured if they’re treated before they have a chance to spread. This emphasizes the crucial role of early detection. The earlier skin cancer is found and removed, the better the chances of a full recovery. It’s essential to schedule regular check-ups with a dermatologist to ensure that any potential issues are identified promptly. If you notice something unusual on your skin, don’t hesitate to contact your doctor.
Types of Skin Cancer
As noted by the Cancer Research UK, different types of skin cancer have varying prognoses:
Basal cell carcinoma (BCC)
BCC is highly curable, with an extremely low likelihood of spreading to other parts of the body. Most cases can be treated effectively by removing the cancerous tissue along with a small margin of surrounding healthy skin.
Squamous Cell Carcinoma (SCC)
SCC is also typically curable, with a high success rate in treatment. In some instances where SCC has spread to lymph nodes or other parts of the body, it may still be curable through appropriate treatment such as surgery, radiation therapy, targeted therapy, or cryotherapy.[2]
Melanoma
Early stage melanoma is often curable through surgery.[3] Among the surgical techniques available for melanoma, wide excision is commonly recommended. This procedure involves the complete removal of the cancerous tissue. More advanced melanoma will often require additional forms of treatment, such a s lymph node dissections, immunotherapy and targeted therapy.
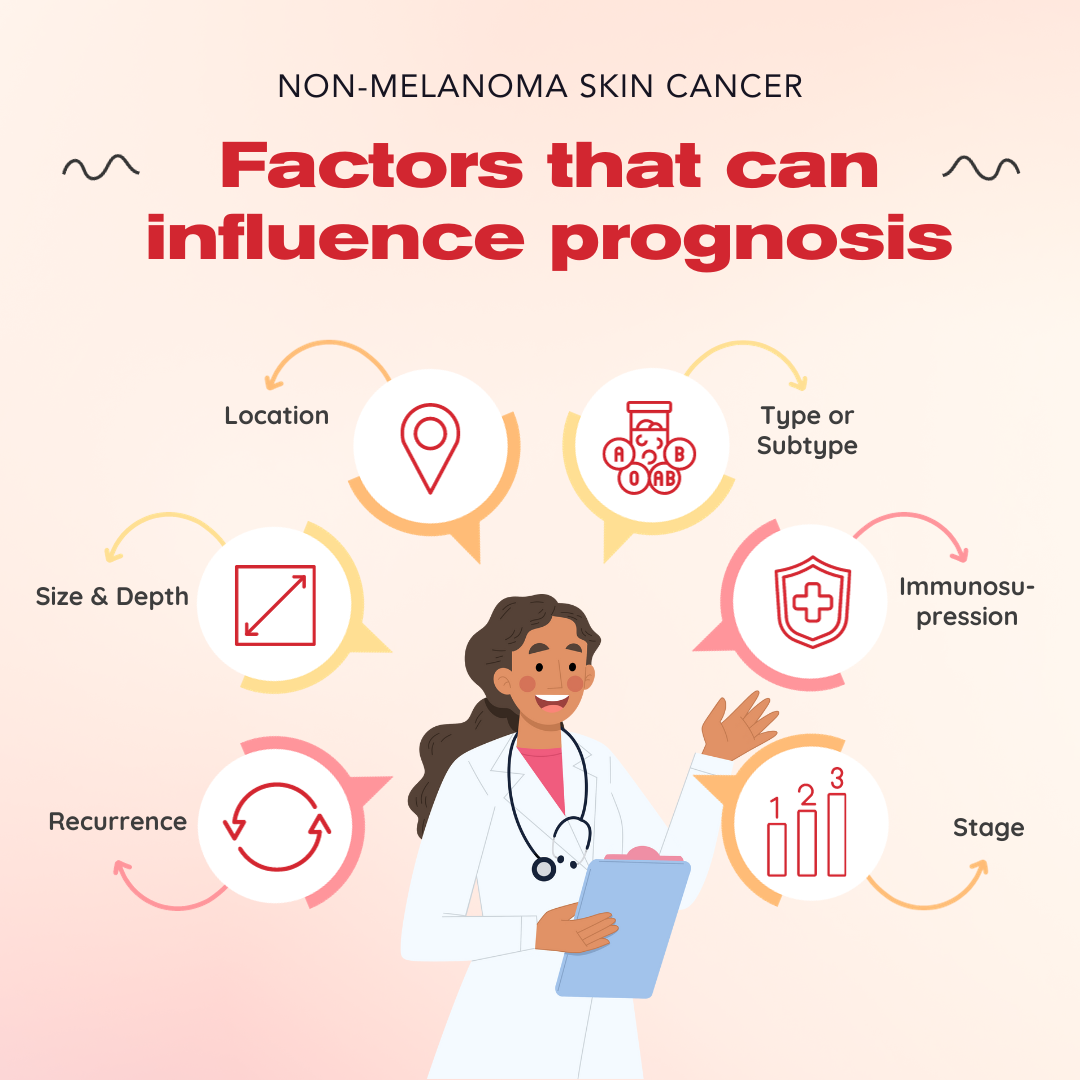
Prognostic Factors
The prognosis for non-melanoma skin cancers is generally excellent, but various factors can influence the outcome, as explained by the Canadian Cancer Society. These factors include:
Location: Skin cancer on certain areas, such as around the eyes, nose, lips, ears, scalp, fingers, toes, and genitals, may have a higher risk of recurrence or metastasis.
Size and Depth: Larger tumors and those that have grown deep into the skin are more likely to come back.
Recurrence: Skin cancer that returns after treatment may have a less favorable prognosis.
Type or Subtype: Some subtypes of BCC and SCC tend to grow more quickly and have different outcomes.
Immunosuppression: Weakened immune systems can impact the prognosis.
Stage: The stage at diagnosis is a significant determinant of prognosis.
Is Skin Cancer Curable?
In general, the outlook for skin cancer is positive. The 5-year survival rate for melanoma is 99% if detected and treated before it spreads to the lymph nodes, according to the American Academy of Dermatology. For BCC and SCC, the outlook is favorable, especially when diagnosed early. However, as skin cancer advances, the prognosis may vary.
In conclusion, most skin cancers are curable, especially when detected and treated in their early stages. Early detection, regular check-ups with a dermatologist, and prompt treatment are essential in ensuring a positive outcome. While skin cancer can be a serious diagnosis, advances in medical treatments offer hope and optimism for those affected by this condition.
Please remember that the statistics and opinions cited on this page are general, and do not apply to every person’s experience of skin cancer. And if you have concerns about your specific case, consult with your healthcare provider for personalized guidance on your prognosis and treatment options.
[1] “Skin Cancer.” Canadian Skin Cancer Foundation, www.canadianskincancerfoundation.com/skin-cancer/. Accessed 9 Oct. 2023.
[2] “Is Skin Cancer Curable.” Medical News Today, www.medicalnewstoday.com/articles/is-skin-cancer-curable. Accessed 9 Oct. 2023.
[3] “Melanoma Overview.” Skin Cancer Foundation, www.skincancer.org/skin-cancer-information/melanoma/. Accessed 9 Oct. 2023.


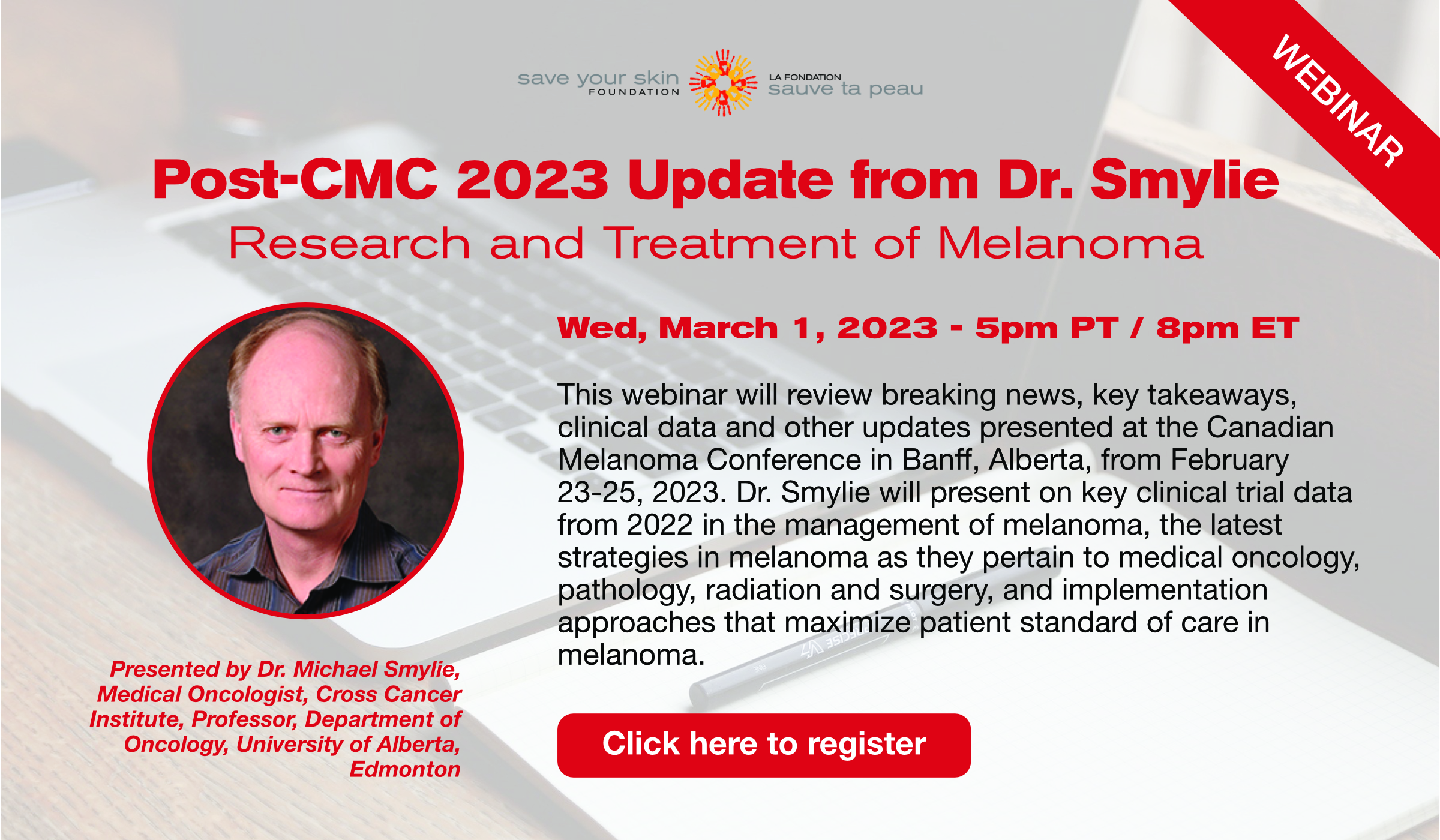 Date/Time: March 1 – 5pm-6:30 pm PT / 8pm-9:30 pm ET
Date/Time: March 1 – 5pm-6:30 pm PT / 8pm-9:30 pm ET