Better Pharmacare Coalition eager to work with government to get it right for patients
VANCOUVER, Feb. 9, 2016 /CNW/ – A recent Better Pharmacare Coalition (BPC) poll1 has found that British Columbians oppose expansion of the Ministry of Health’s Reference Drug Program based on concerns that expansion could compromise patient health.
The BC government has approved amendments to the Drug Price Regulation that will expand the Ministry of Health’s Reference Drug Program (RDP). In anticipation of this expansion, the BPC conducted an online poll, which found a resounding 82% of British Columbians are concerned that administrators of the BC PharmaCare program will be implementing a policy that tells physicians which medications they can prescribe for patients, even if it goes against physicians’ opinions of the best care for their patients.
“We are very concerned about senior and low-income patients’ health with the expansion of the Reference Drug Program as they are typically the first to feel the negative consequences of policy reform. When the BC government’s planned policy is enacted, these vulnerable individuals and other patients relying on BC PharmaCare will not be able to afford their current medication, medication that is keeping them well or from declining health,” said Cheryl Koehn, BPC founding member and president of Arthritis Consumer Experts. “Changing a medication in a stabilized patient strictly based on an expanded government pricing scheme is contrary to best practice in today’s policy development environment. We fully support a “patients first” approach and so should governments. Policy should preserve and uphold the health care system’s desire to deliver precision medicine.”
Starting June 1, 2016, the BC government will create three new reference drug categories – Angiotensin Receptor Blocker (reduces high blood pressure), Proton Pump Inhibitor (treats GERD/heartburn), and Statin (lowers cholesterol) – and begin transitioning patients from one to another medication in these groups, which could immediately put their health at risk. By December 1, 2016, the new policy will be in effect.
The BPC poll also found that 76% of British Columbians were concerned about changing BC PharmaCare’s Reference Drug Program to specify a ‘reference product’ that patients must take, or they will have to pay the difference out-of-pocket to stay on their current therapy. It is important to note that the concerns are higher among PharmaCare users and those with a history of chronic disease in their household.
“The BPC has been clear from its inception and through consultations with the BC government’s Pharmaceutical Task Force, that Reference Drug Program expansion will reduce quality health care at the individual level. An economic study,2 conducted after RDP was introduced in BC in 1995, revealed that the policy pushed costs to other parts of the health care system, generated negative health outcomes for the elderly and low income patients.
A 2009 study led by the Canadian Society of Intestinal Research3 showed that changing medication against doctor’s orders, which BC PharmaCare predicted would preserve $42 million in the drug budget, actually cost the BC government $43 million more, a difference of $85 million for BC,” said Gail Attara, BPC member and CEO of the Gastrointestinal Society.
“The government needs to understand what doctors already know – patients are unique and they cannot be treated with a cookie cutter approach. Government should make every effort to meaningfully consult with our coalition’s members when contemplating any change that will touch even one patient’s life. We are ready, willing, and able to work by their sides to get it right for BC patients,” added Attara.
About Better Pharmacare Coalition
The Better Pharmacare Coalition was formed in 1997 in response to BC PharmaCare policy development not being reflective of current medical literature, best clinical practices and the needs of patients in BC. The coalition works together to call for appropriate access to evidence-based medicines that are proved effective and needed by patients in BC. The member organizations include: Arthritis Consumer Experts, Atypical Hemolytic Uremic Syndrome Canada, BC Lung Association, BC Schizophrenia Society, British Columbia Coalition of Osteoporosis Physicians, Canadian Arthritis Patient Alliance, Canadian Society of Intestinal Research, Canadian Osteoporosis Patient Network, Crohn’s and Colitis Canada; Gastrointestinal Society, Kidney Foundation of Canada, Mood Disorders Association of British Columbia, MS Society of Canada, BC Division, Pacific Hepatitis C Network of BC, Parkinson Society British Columbia, Prostate Cancer Foundation BC, Save your Skin Foundation, and The Arthritis Society, BC and Yukon Division. More information is available online at www.betterpharmacare.org.
_______________________________
1 BPC engaged Insights West to conduct an online survey in December 2015 to determine British Columbians’ opinions on BC PharmaCare and in particular their opinions on the expansion of the Reference Drug Program. Results are based on an online study among 858 adult British Columbians. The data has been statistically weighted according to Canadian census figures for age, gender and region. The margin of error (which measures sample variability) is ±3.4 percentage points.
2 Aslam Anis. Why is calling an ACE an ACE so controversial? Evaluating reference-based pricing in British Columbia. Canadian Medical Association Journal. 2002; 166(6):763-764.
3 Skinner BJ, Gray JR, Attara GP. Increased health costs from mandated Therapeutic Substitution of proton pump inhibitors in British Columbia. Alimentary Pharmacology and Therapeutics. 2009;29(8):882–891.
SOURCE Arthritis Consumer Experts
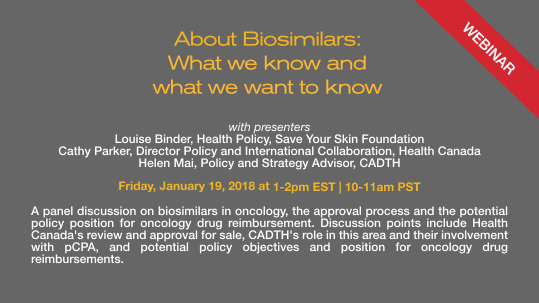
Image with caption: “Patient Poll on RDP (CNW Group/Arthritis Consumer Experts)”. Image available at:http://photos.newswire.ca/images/download/20160209_C7043_PHOTO_EN_616353.jpg 
For further information: Kelly Lendvoy, Vice President, Communications & Public Affairs, Arthritis Consumer Experts, 604.379.9898