PHYSICAL EXAMS FOR SKIN CANCER SCREENING: WHAT IT IS AND HOW TO PREPARE
Written by Megan Lam
Medicine, McMaster University
Class of 2022
Early detection of skin cancers is vital, and skin cancer screening exams performed by health care professionals can help to catch suspicious moles and marks early. While most skin cancers develop on areas of skin that are often exposed to sun, skin cancers can still occur on areas that aren’t always exposed to sun, such as in folds and in between digits [1]. Melanoma, the most deadly type of skin cancer, accounts for almost 4% of new cancer cases in Canada, and over 1 in 8 Canadians will develop a non-melanoma skin cancer in their lifetime, according to the government of Canada [2]. Skin cancer screenings can not only help diagnose skin cancers, your healthcare provider can also identify pre-cancerous changes in your skin and treat those areas before they become cancerous.
Cancerous and pre-cancerous lesions that can be identified by skin cancer screenings include:
- Actinic keratosis (AK): A common precancerous skin condition, they typically develop on areas with prolonged sun exposure such as the arms, head and neck, and may present as scaly or thickened areas.
- Squamous cell carcinoma (SCC): Actinic keratoses may predispose patients to developing SCC, which is the 2nd most common type of skin cancer and may look like scaly patches or recurrent sores.
- Basal cell carcinoma (BCC): The most common type of skin cancer, BCC typically presents as a pearly or skin-coloured bump.
- Melanoma: Melanomas are the most dangerous type of skin cancer and the most likely type to metastasize.
PREPARING FOR YOUR EXAM
- Before arriving, make note of any new, or unusual spots, as well as photos of any spots that appear to have changed over time;
- Be ready to remove your clothing before your exam and limit wearing accessories such as heavy bracelets and watches as these may have to be removed as well;
- Remove any make-up or nail polish that may be hiding any suspicious spots on the face or under the nails;
- Your health care provider will also be examining your scalp, so having your hair down and removing any hair clips, pony tails, or buns before-hand will be helpful.
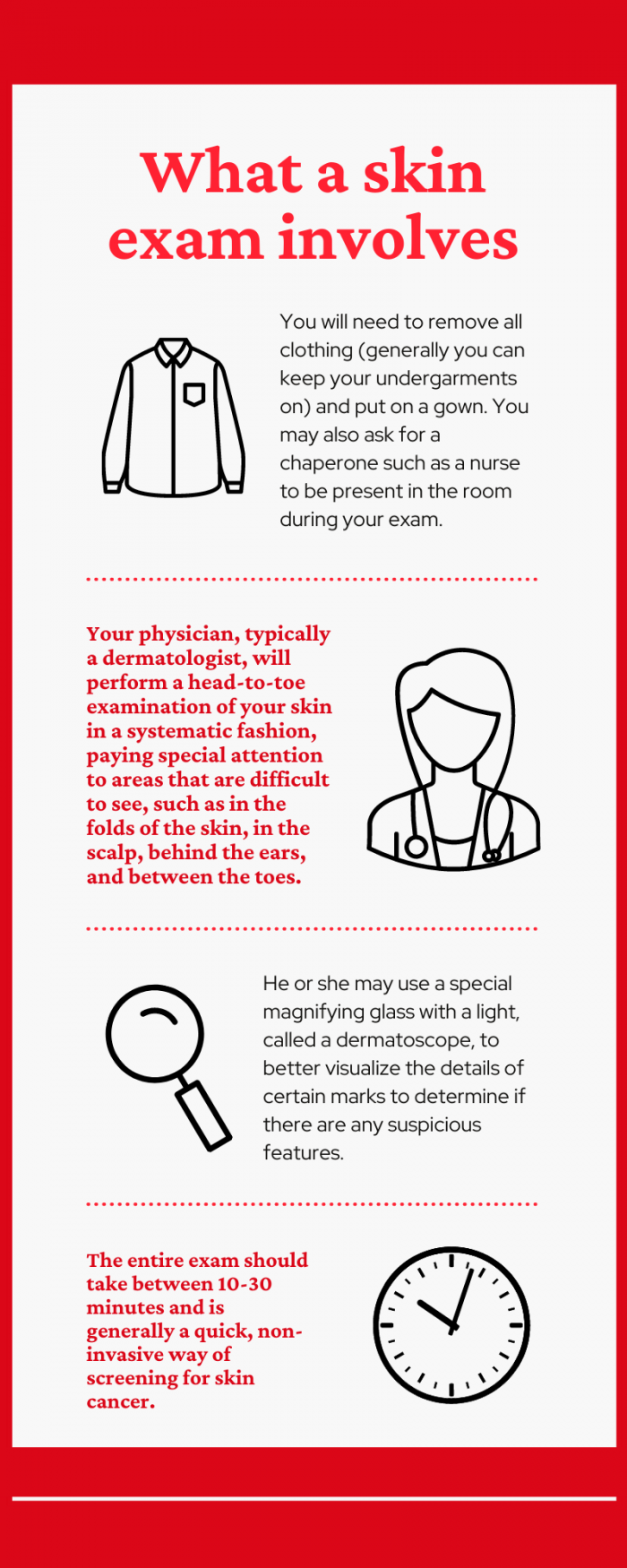
WHAT YOUR EXAM INVOLVES
You will need to remove all clothing (generally you can keep your undergarments on) and put on a gown. You may also ask for a chaperone such as a nurse to be present in the room during your exam. Your physician, typically a dermatologist, will perform a head-to-toe examination of your skin in a systematic fashion, paying special attention to areas that are difficult to see, such as in the folds of the skin, in the scalp, behind the ears, and between the toes. He or she may use a special magnifying glass with a light, called a dermatoscope, to better visualize the details of certain marks to determine if there are any suspicious features. The entire exam should take between 10-30 minutes and is generally a quick, non-invasive way of screening for skin cancer.
FROM YOUR HEALTH CARE PROVIDER’S PERSPECTIVE
Health care providers will look for certain suspicious features, in particular, for any dark spots that may be melanoma. The features that they look for follow the ABCDE rule:
- Asymmetry: an irregular or asymmetrical shape
- Border: blurred, ragged or broken borders
- Colour: many different colours within a single mole
- Diameter: larger than 6 mm in diameter
- Evolution: changing in size, shape or colour
Your healthcare provider may opt to simply watch and wait for cancerous change in the case of moles or marks that appear low risk. However, for any suspicious areas, a biopsy may be taken, which involves the removal of a small skin sample. Usually the skin around the area will be frozen with lidocaine so you will hardly feel it. Afterwards, the skin sample is sent to a lab or examined more closely under a microscope for cancer cells. Small lesions that are suspicious can occasionally be completely excised during the biopsy, although an additional excision may need to be performed in order to ensure adequate margins are removed around the lesion.
FOLLOWING UP AFTER YOUR SKIN EXAM
Your health care provider will likely contact you or your family doctor if the results of the biopsy showed suspicious, precancerous, or cancerous changes. If a suspicious mole or mark was found but no biopsy was taken, your health care provider may elect to monitor and follow-up within an appropriate timeframe to re-examine for any changes. If there were no suspicious findings, annual or sometimes bi-annual screenings are recommended. Those at higher risk may need to be examined more often, such as individuals with a large number of moles or freckles, significant UV or sun exposure, a personal history of skin cancer, or light-coloured skin, hair or eyes. The sooner a skin cancer lesion can be identified, the more treatment options and the more effective treatment will be.
REFERENCES
[1] Juzeniene A, Baturaite Z, Moan J. Cutaneous malignant melanoma incidence rates in Norway. In: Reichrath J, editor. Sunlight, Vitam. D Ski. Cancer. 2nd ed., Landes Bioscience and Springer Science+Business Media; 2013. https://doi.org/10.1177/1403494813479216.
[3] Stern RS. Prevalence of a history of skin cancer in 2007: Results of an incidence-based model. Arch Dermatol 2010;146:279–82. https://doi.org/10.1001/archdermatol.2010.4.
NOTE: The information on the Save Your Skin website is not intended to replace the medical advice of a doctor or healthcare provider. While we make every effort to ensure that the information on our site is as current as possible, please note that information and statistics are subject to change as new research and studies are published.
MONTHLY SELF-EXAMS ARE KEY TO EARLY DETECTION
Making awareness and education available is crucial. Since 2006, the Foundation has worked to raise awareness of melanoma and non-melanoma skin cancers focusing on education, prevention and the need for improved patient care.